Search
- Page Path
- HOME > Search
Review Article
- Miscellaneous
- Quality Matters as Much as Quantity of Skeletal Muscle: Clinical Implications of Myosteatosis in Cardiometabolic Health
- Hong-Kyu Kim, Chul-Hee Kim
- Endocrinol Metab. 2021;36(6):1161-1174. Published online December 28, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1348

- 6,461 View
- 284 Download
- 27 Web of Science
- 29 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Although age-related changes in skeletal muscles are closely associated with decreases in muscle strength and functional decline, their associations with cardiometabolic diseases in the literature are inconsistent. Such inconsistency could be explained by the fact that muscle quality—which is closely associated with fatty infiltration of the muscle (i.e., myosteatosis)—is as important as muscle quantity in cardiometabolic health. However, muscle quality has been less explored compared with muscle mass. Moreover, the standard definition of myosteatosis and its assessment methods have not been established yet. Recently, some techniques using single axial computed tomography (CT) images have been introduced and utilized in many studies, as the mass and quality of abdominal muscles could be measured opportunistically on abdominal CT scans obtained during routine clinical care. Yet, the mechanisms by which myosteatosis affect metabolic and cardiovascular health remain largely unknown. In this review, we explore the recent advances in the assessment of myosteatosis and its changes associated with aging. We also review the recent literature on the clinical implication of myosteatosis by focusing on metabolic and cardiovascular diseases. Finally, we discuss the challenges and unanswered questions that need addressing to set myosteatosis as a therapeutic target for the prevention or treatment of cardiometabolic diseases.
-
Citations
Citations to this article as recorded by- A CT-based Deep Learning Model for Predicting Subsequent Fracture Risk in Patients with Hip Fracture
Yisak Kim, Young-Gon Kim, Jung-Wee Park, Byung Woo Kim, Youmin Shin, Sung Hye Kong, Jung Hee Kim, Young-Kyun Lee, Sang Wan Kim, Chan Soo Shin
Radiology.2024;[Epub] CrossRef - Myosteatosis is associated with poor survival after kidney transplantation: a large retrospective cohort validation
Jie Chen, Yue Li, Chengjie Li, Turun Song
Abdominal Radiology.2024; 49(4): 1210. CrossRef - Fatty infiltration of gastrocnemius–soleus muscle complex: Considerations for myosteatosis rehabilitation
Catherine Hatzantonis, Lalith Satkunam, Karyne N. Rabey, Jennifer C. Hocking, Anne M. R. Agur
Journal of Anatomy.2024;[Epub] CrossRef - Muscle attenuation, not skeletal muscle index, is an independent prognostic factor for survival in gastric cancer patients with overweight and obesity
Cheng-Le Zhuang, Hao-Fan Wu, Hao-Jie Jiang, Feng-Min Zhang, Han-Ping Shi, Zhen Yu, Xian Shen, Xiao-Lei Chen, Su-Lin Wang
Nutrition.2024; 122: 112391. CrossRef - Myosteatosis is associated with coronary artery calcification in patients with type 2 diabetes
Fu-Peng Liu, Mu-Jie Guo, Qing Yang, Yan-Ying Li, Yan-Gang Wang, Mei Zhang
World Journal of Diabetes.2024; 15(3): 429. CrossRef - Unlocking liver health: Can tackling myosteatosis spark remission in metabolic dysfunction‐associated steatotic liver disease?
Guillaume Henin, Audrey Loumaye, Louise Deldicque, Isabelle A. Leclercq, Nicolas Lanthier
Liver International.2024;[Epub] CrossRef - Association of serum gamma-glutamyl transferase with myosteatosis assessed by muscle quality mapping using abdominal computed tomography
Han Na Jung, Yun Kyung Cho, Hwi Seung Kim, Eun Hee Kim, Min Jung Lee, Joong-Yeol Park, Woo Je Lee, Hong-Kyu Kim, Chang Hee Jung
Clinical Imaging.2023; 93: 4. CrossRef - Increased visceral fat area to skeletal muscle mass ratio is positively associated with the risk of cardiometabolic diseases in a Chinese natural population: A cross‐sectional study
Shi Zhang, Yaping Huang, Jing Li, Xincheng Wang, Xiaohe Wang, Minying Zhang, Yanju Zhang, Meiyang Du, Jingna Lin, Chunjun Li
Diabetes/Metabolism Research and Reviews.2023;[Epub] CrossRef - Association between hypertension and myosteatosis evaluated by abdominal computed tomography
Han Na Jung, Yun Kyung Cho, Hwi Seung Kim, Eun Hee Kim, Min Jung Lee, Woo Je Lee, Hong-Kyu Kim, Chang Hee Jung
Hypertension Research.2023; 46(4): 845. CrossRef - Epidemiological, mechanistic, and practical bases for assessment of cardiorespiratory fitness and muscle status in adults in healthcare settings
Jaime A. Gallo-Villegas, Juan C. Calderón
European Journal of Applied Physiology.2023; 123(5): 945. CrossRef - Muscle fat infiltration in chronic kidney disease: a marker related to muscle quality, muscle strength and sarcopenia
Carla Maria Avesani, Aline Miroski de Abreu, Heitor S. Ribeiro, Torkel B. Brismar, Peter Stenvinkel, Alice Sabatino, Bengt Lindholm
Journal of Nephrology.2023; 36(3): 895. CrossRef - IDF2022-1139 Association Between Dyslipidemia And Myosteatosis Using Visual Muscular Quality Map In Computed Tomography
H.S. Kim, H.N. Jung, Y.K. Cho, E.H. Kim, M.J. Lee, W.J. Lee, J.Y. Park, H.K. Kim, C.H. Jung
Diabetes Research and Clinical Practice.2023; 197: 110467. CrossRef - The role of skeletal muscle mass on cardiovascular disease risk: an emerging role on modulating lipid profile
Evangelia Damigou, Matina Kouvari, Demosthenes Panagiotakos
Current Opinion in Cardiology.2023; 38(4): 352. CrossRef - Reference values for low muscle mass and myosteatosis using tomographic muscle measurements in living kidney donors
Lisa B. Westenberg, Marcel Zorgdrager, Tim D. A. Swaab, Marco van Londen, Stephan J. L. Bakker, Henri G. D. Leuvenink, Alain R. Viddeleer, Robert A. Pol
Scientific Reports.2023;[Epub] CrossRef - Association between sarcopenic obesity and poor muscle quality based on muscle quality map and abdominal computed tomography
Yun Kyung Cho, Han Na Jung, Eun Hee Kim, Min Jung Lee, Joong‐Yeol Park, Woo Je Lee, Hong‐Kyu Kim, Chang Hee Jung
Obesity.2023; 31(6): 1547. CrossRef - Increase in skeletal muscular adiposity and cognitive decline in a biracial cohort of older men and women
Caterina Rosano, Anne Newman, Adam Santanasto, Xiaonan Zhu, Bret Goodpaster, Iva Miljkovic
Journal of the American Geriatrics Society.2023; 71(9): 2759. CrossRef - Evaluation of Paraspinal Muscle Degeneration on Pain Relief after Percutaneous Epidural Adhesiolysis in Patients with Degenerative Lumbar Spinal Disease
Misun Kang, Shin Hyung Kim, Minju Jo, Hyun Eom Jung, Jungbin Bae, Hee Jung Kim
Medicina.2023; 59(6): 1118. CrossRef - Sarcopenic obesity and its relation with muscle quality and mortality in patients on chronic hemodialysis
Alice Sabatino, Carla Maria Avesani, Giuseppe Regolisti, Marianna Adinolfi, Giuseppe Benigno, Marco Delsante, Enrico Fiaccadori, Ilaria Gandolfini
Clinical Nutrition.2023; 42(8): 1359. CrossRef - Association between computed tomography‐assessed sarcopenia and mortality in patients with anti‐neutrophil cytoplasmic antibody‐associated vasculitis
Sung Soo Ahn, Yong‐Beom Park, Sang‐Won Lee
International Journal of Rheumatic Diseases.2023; 26(9): 1704. CrossRef - Association Between Insulin Resistance and Myosteatosis Measured by Abdominal Computed Tomography
Myung Jin Kim, Yun Kyung Cho, Han Na Jung, Eun Hee Kim, Min Jung Lee, Chang Hee Jung, Joong-Yeol Park, Hong-Kyu Kim, Woo Je Lee
The Journal of Clinical Endocrinology & Metabolism.2023; 108(12): 3100. CrossRef - Association of Visceral Fat Obesity, Sarcopenia, and Myosteatosis with Non-Alcoholic Fatty Liver Disease without Obesity
Hong-Kyu Kim, Sung-Jin Bae, Min Jung Lee, Eun Hee Kim, Hana Park, Hwi Seung Kim, Yun Kyung Cho, Chang Hee Jung, Woo Je Lee, Jaewon Choe
Clinical and Molecular Hepatology.2023; 29(4): 987. CrossRef - Different computed tomography parameters for defining myosteatosis in patients with advanced non-small cell lung cancer
Wenyi Zhang, Jing Tang, Huiyu Tang, Lingling Xie, Jing Wang, Jinhui Wu, Ming Yang
Clinical Nutrition.2023; 42(12): 2414. CrossRef - All you need to know about sarcopenia: a short guide for an internal medicine physician in questions and answers
G. R. Bikbavova, M. A. Livzan, D. V. Tikhonravova
Bulletin of Siberian Medicine.2023; 22(3): 88. CrossRef - Muscle Fat Content Is Associated with Nonalcoholic Fatty Liver Disease and Liver Fibrosis in Chinese Adults
W. Guo, X. Zhao, D. Cheng, X. Liang, M. Miao, X. Li, J. Lu, N. Xu, Shuang Hu, Qun Zhang
The Journal of nutrition, health and aging.2023; 27(11): 960. CrossRef - Body Composition Evaluation and Clinical Markers of Cardiometabolic Risk in Patients with Phenylketonuria
Luis M. Luengo-Pérez, Mercedes Fernández-Bueso, Ana Ambrojo, Marta Guijarro, Ana Cristina Ferreira, Luís Pereira-da-Silva, André Moreira-Rosário, Ana Faria, Conceição Calhau, Anne Daly, Anita MacDonald, Júlio César Rocha
Nutrients.2023; 15(24): 5133. CrossRef - Assessment of Muscle Quantity, Quality and Function
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2022; 31(1): 9. CrossRef - Influence of cross‐sectional area and fat infiltration of paraspinal muscles on analgesic efficacy of epidural steroid injection in elderly patients
Hee Jung Kim, Miribi Rho, Kyung Bong Yoon, Minju Jo, Dong Woo Lee, Shin Hyung Kim
Pain Practice.2022; 22(7): 621. CrossRef - Sarcopenia, Obesity, Sarcopenic Obesity and Risk of Poor Nutritional Status in Polish Community-Dwelling Older People Aged 60 Years and Over
Marika Murawiak, Roma Krzymińska-Siemaszko, Aleksandra Kaluźniak-Szymanowska, Marta Lewandowicz, Sławomir Tobis, Katarzyna Wieczorowska-Tobis, Ewa Deskur-Śmielecka
Nutrients.2022; 14(14): 2889. CrossRef - Metabolic mechanisms for and treatment of NAFLD or NASH occurring after liver transplantation
Amedeo Lonardo, Alessandro Mantovani, Salvatore Petta, Amedeo Carraro, Christopher D. Byrne, Giovanni Targher
Nature Reviews Endocrinology.2022; 18(10): 638. CrossRef
- A CT-based Deep Learning Model for Predicting Subsequent Fracture Risk in Patients with Hip Fracture

Original Articles
- Diabetes, Obesity and Metabolism
- Prognostic Value of Triglyceride and Glucose Index for Incident Type 2 Diabetes beyond Metabolic Health and Obesity
- Hwi Seung Kim, Jiwoo Lee, Yun Kyung Cho, Eun Hee Kim, Min Jung Lee, Hong-Kyu Kim, Joong-Yeol Park, Woo Je Lee, Chang Hee Jung
- Endocrinol Metab. 2021;36(5):1042-1054. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1184
- 5,349 View
- 133 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
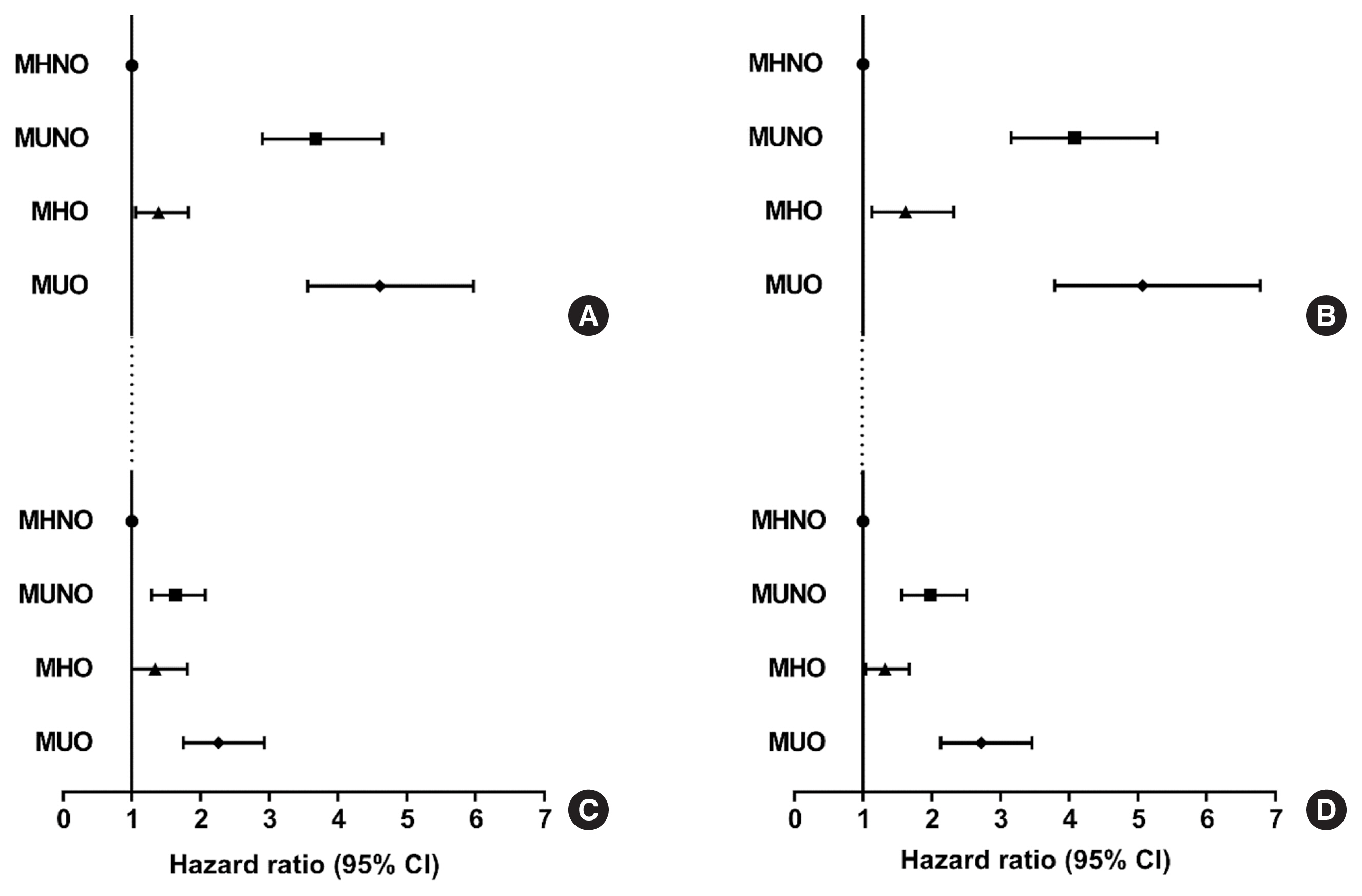
Metabolically healthy obese (MHO) phenotype is metabolically heterogeneous in terms of type 2 diabetes (T2D). Previously, the triglyceride and glucose (TyG) index has been considered for identifying metabolic health and future risk of T2D. This study aimed to evaluate the risk of incident T2D according to obesity status and metabolic health, categorized by four different criteria and the TyG index.
Methods
The study included 39,418 Koreans without T2D at baseline. The risk of T2D was evaluated based on four different definitions of metabolic health and obesity status and according to the baseline TyG index within each metabolic health and obesity group.
Results
During the median follow-up at 38.1 months, 726 individuals developed T2D. Compared with the metabolically healthy non-obese (MHNO) group with low TyG index, the MHO group with high TyG index showed increased risk of T2D in all four definitions of metabolic health with multivariate-adjusted hazard ratios of 2.57 (95% confidence interval [CI], 1.76 to 3.75), 3.72 (95% CI, 2.15 to 6.43), 4.13 (95% CI, 2.67 to 6.38), and 3.05 (95% CI, 2.24 to 4.15), when defined by Adult Treatment Panel III, Wildman, Karelis, and homeostasis model assessment (HOMA) criteria, respectively.
Conclusion
MHO subjects with high TyG index were at an increased risk of developing T2D compared with MHNO subjects, regardless of the definition of metabolic health. TyG index may serve as an additional factor for predicting the individual risk of incident T2D in MHO subjects.

- Clinical Study
- Gender-Dependent Reference Range of Serum Calcitonin Levels in Healthy Korean Adults
- Eyun Song, Min Ji Jeon, Hye Jin Yoo, Sung Jin Bae, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Hong-Kyu Kim, Won Gu Kim
- Endocrinol Metab. 2021;36(2):365-373. Published online April 7, 2021
- DOI: https://doi.org/10.3803/EnM.2020.939

- 5,055 View
- 152 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Serum calcitonin measurement contains various clinical and methodological aspects. Its reference level is wide and unclear despite sensitive calcitonin kits are available. This study aimed to identify the specific reference range in the healthy Korean adults.
Methods
Subjects were ≥20 years with available calcitonin (measured by a two-site immunoradiometric assay) data by a routine health checkup. Three groups were defined as all eligible subjects (group 1, n=10,566); subjects without self or family history of thyroid disease (group 2, n=5,152); and subjects without chronic kidney disease, autoimmune thyroid disease, medication of proton pump inhibitor/H2 blocker/steroid, or other malignancies (group 3, n=4,638).
Results
This study included 6,341 male and 4,225 female subjects. Males had higher mean calcitonin than females (2.3 pg/mL vs. 1.9 pg/mL, P<0.001) in group 1. This gender difference remained similar in groups 2 and 3. Calcitonin according to age or body mass index was not significant in both genders. Higher calcitonin in smoking than nonsmoking men was observed but not in women. Sixty-nine subjects had calcitonin higher than the upper reference limit (10 pg/mL) and 64 of them had factors associated with hypercalcitoninemia besides medullary thyroid cancer. Our study suggests the reference intervals for men who were non, ex-, current smokers, and women (irrespective of smoking status) as <5.7, <7.1, <7.9, and <3.6 pg/mL, respectively.
Conclusion
Specific calcitonin reference range should be provided considering for sex and smoking status. Taking account for several factors known to induce hypercalcitoninemia can help interpret the gray zone of moderately elevated calcitonin. -
Citations
Citations to this article as recorded by- Determinants of circulating calcitonin value: analysis of thyroid features, demographic data, anthropometric characteristics, comorbidities, medications, and smoking habits in a population with histological full exclusion of medullary thyroid carcinoma
Pierpaolo Trimboli, Giuseppe Peloni, Dorotea Confalonieri, Elena Gamarra, Tommaso Piticchio, Francesco Frasca, Petra Makovac, Arnoldo Piccardo, Lorenzo Ruinelli
Frontiers in Oncology.2024;[Epub] CrossRef - Surgical treatment of solid variant of papillary thyroid carcinoma: Fifteen-year experience of a tertiary center
Katarina Tausanović, Marina Stojanović, Milan Jovanović, Boban Stepanović, Jovan Ilić, Sara Ivaniš, Vladan Živaljević
Medicinska istrazivanja.2024; 57(1): 121. CrossRef - Some genetic differences in patients with rheumatoid arthritis
Hosam M. Ahmad, Zaki M. Zaki, Asmaa S. Mohamed, Amr E. Ahmed
BMC Research Notes.2023;[Epub] CrossRef - Presence or severity of Hashimoto’s thyroiditis does not influence basal calcitonin levels: observations from CROHT biobank
M. Cvek, A. Punda, M. Brekalo, M. Plosnić, A. Barić, D. Kaličanin, L. Brčić, M. Vuletić, I. Gunjača, V. Torlak Lovrić, V. Škrabić, V. Boraska Perica
Journal of Endocrinological Investigation.2022; 45(3): 597. CrossRef - Environmental Factors That Affect Parathyroid Hormone and Calcitonin Levels
Mirjana Babić Leko, Nikolina Pleić, Ivana Gunjača, Tatijana Zemunik
International Journal of Molecular Sciences.2021; 23(1): 44. CrossRef
- Determinants of circulating calcitonin value: analysis of thyroid features, demographic data, anthropometric characteristics, comorbidities, medications, and smoking habits in a population with histological full exclusion of medullary thyroid carcinoma


 KES
KES

 First
First Prev
Prev



